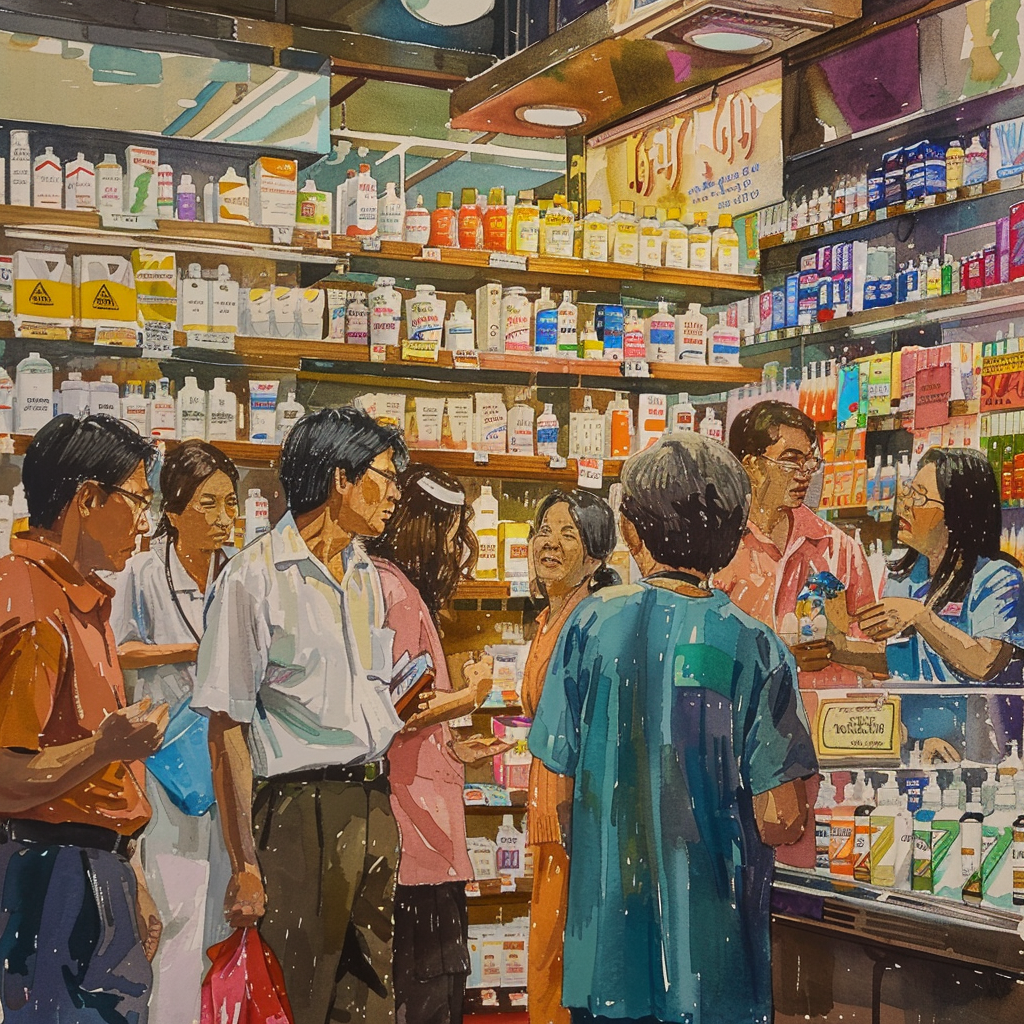
Amid the bustling scene at a Government Pharmaceutical Organization outlet on Rama VI Road in Bangkok’s vibrant Ratchathewi district, a serious debate is brewing, much to the chagrin of shoppers. It’s a classic case of a civil society group pitted against a medical authority. The bone of contention? The Medical Council of Thailand’s decision to take legal action against the National Health Security Office (NHSO)’s policy of providing free medicine for 16 common ailments under the universal healthcare scheme.
Saree Aongsomwang, the charismatic secretary-general of the Thailand Consumer Council (TCC), made waves on Saturday. She voiced her concerns about the ongoing dispute, which transcends mere bureaucratic wrangling to touch the very nerve of patient welfare. The Supreme Administrative Court had just agreed to hear the Medical Council’s complaint, marking a potential turning point. This issue wrestles with free access to medicine at pharmacies, tackling everyday symptoms like headaches, joint pain, and coughs, without which patients may end up more sick, or so argue the policy’s defenders.
Initiated in 2022, the free-medicine policy already boasts a solid following. According to supporters, it’s a literal lifesaver—scratching the itch of overcrowding in hospitals and lightening the load for healthcare workers. Saree and her allies argue that it fits neatly into the Ministry of Public Health’s blueprint to reinforce primary healthcare’s frontline capabilities. Importantly, it empowers patients with options: receive medicine at a pharmacy or opt for a traditional hospital visit.
“This legal maneuver has sowed seeds of confusion among consumers who dread the day this service sees its last,” Saree lamented. Her call to action is clear—a retreat on the lawsuit. The goal? Forge a pact that benefits the one crucial stakeholder: patients.
Despite the courtroom theatrics, NHSO deputy secretary-general Dr. Attaporn Limpanyalert offers a steady hand of reassurance. He asserts that universal healthcare cardholders will continue to benefit from the scheme until the court has its final say.
Adding to the narrative, the Pharmacy Council of Thailand underscores the diligence of pharmacists, noting that over 1.79 million people have taken advantage of the policy since its rollout in October 2022. In fact, 90% have shaken off their symptoms, and there are no harrowing tales of adverse effects.
The Pharmacy Council’s stance is intriguing—they perceive no qualms from the Medical Council when individuals independently purchase their medications. The bone of contention, they note, is solely the free medicine for universal healthcare card holders. Cynics may smell a rat, questioning if medical safety is the sole concern.
With a call to action as weighty as an elephant’s stomp, the Pharmacy Council urges its counterpart to honor the professional ethics that underscore the delicate art and science of prescriptions.
As the drama unfolds, one can’t help but muse over what’s at stake. At the heart of this debate lies the shared belief in enhancing the public’s health and ensuring it isn’t encumbered by boardroom battles. For Bangkok’s medical shoppers and patients all across Thailand, the resolution cannot come soon enough.















It’s ridiculous that the Medical Council is trying to block free medicine. People should have access to medication without jumping through hoops!
But without regulation, who ensures the quality and safety of these free medications?
Quality is crucial, but the Pharmacy Council has reported no issues so far. It seems like a non-issue.
Free doesn’t mean unsafe. Regulations still apply in a universal healthcare setup.
I think the real issue here is whether the NHSO can maintain funding if the free medicine program grows. Money doesn’t grow on trees!
As a healthcare professional, I am concerned about self-medication risks. Patients might misuse drugs when not supervised.
Isn’t that what pharmacists are for? They can provide guidance, can’t they?
Pharmacists help, but they’re not doctors. Complex cases need more oversight.
With proper guidelines, pharmacists can handle most routine cases efficiently.
Self-medication is a risk for any country, but that’s where public education plays a role.
The legal battle is more about power than patient care. Who’s really benefiting from this squabble?
Follow the money, always. Who profits if the program is scrapped?
Exactly. The pharmacies and private hospitals stand to gain a lot.
It’s time for Thailand to prioritize universal healthcare. Every citizen deserves access to essential medicines!
Perhaps the solution is compromise: maintain the program, enhance oversight, and ensure medicines’ quality.
Compromise sounds ideal, but will both sides agree to it? That’s the million-dollar question.
It might take external pressure from public opinion to push them towards compromise.
What happens if the court rules in favor of the Medical Council? It’s scary to think about losing this service!
It might lead to protests. People are pretty passionate about their healthcare rights.
Countries with free access to medicines enjoy longer life expectancies. What does Thailand’s Medical Council say about that?
This is classic elitism. Only the rich should afford proper medicine, right? (sarcasm)
Ironically, the rich have no problem paying, but they lobby to keep services from the poor.
We should think about the long-term sustainability of such programs. What happens in an economic downturn?
That’s why proper funding channels need to be established now, not later.
At the end of the day, if the government can’t uphold healthcare rights, it’s failing its people.
I trust that Thai courts will rule in the best interest of public health. Anything less would be a travesty.
I wonder how other countries have successfully implemented free medicine programs without such drama. Seems like we can learn more from them.